By John Patkin
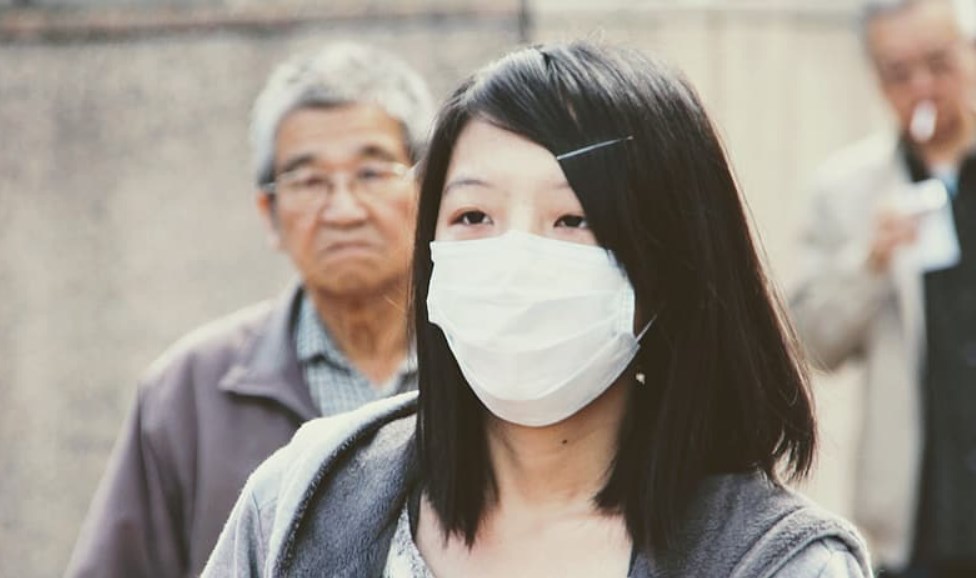
The debate on the efficacy of surgical masks in the prevention of Covid-19 has ignored the underlying reasons why Hongkongers and Asian communities feel the need to cover up in the face of the deadly virus and how they impede oral communication.
The demand for masks is a reaction to 17 years of post-SARS public health education and emblematic of collectivism. Those who experienced SARS and subsequent scares feel morally bound to wear a mask while others who are genuinely concerned about their health get a boost in confidence when they symbolically cover up.
The ubiquity of face masks suggests collective compliance among citizens. But face masks are also an obstacle to effective oral communication, particularly when interlocutors are using a second language.
As a language and communications researcher, I have been fascinated by the challenges I have faced conversing with hospital staff during regular medical check-ups since masks became universal in Hong Kong health care. The inability to decode facial expressions and the absence of lip reading has challenged my ageing hearing.
Without these visual prompts, I am often unsure if someone is talking to me and have to ask them to repeat themselves. This is draining for all parties and may discourage some from discussing important issues.
Despite my misgivings, a post-SARS study investigating the effects of wearing surgical masks during mock senior secondary English oral exams concluded that they did not impede results. But thicker models such as the N95 may lead to a different outcome due to muffling.
A study into the effects of doctors wearing masks found that patients felt there was a lack of empathy but that did not seem to affect clinical outcomes. The authors suggested doctors could focus more on non-verbal behaviour and reflect on oral communication challenges with colleagues.

While both of these studies appear to show minimal communication problems with standard surgical masks, they were limited to samples among the same cultural group, Hong Kong Chinese. Studies of the use of English as a lingua franca among second-language speakers in Hong Kong and South East Asia have shown communication challenges among people who weren’t wearing masks.
If speakers cover their faces, it may amplify communication problems and present intelligibility issues in medical consultations.
Perhaps the area of most concern is the hundreds of thousands of Hong Kong residents who use English as a lingua franca, particularly some groups who are isolated from the mainstream through culture and perceived social ranking. These groups who use English as a second and third language face obstacles when interacting with Cantonese speakers.
Translation services and online advice are available but not always suitable for day-to-day interactions, and not as detailed or current as those in Chinese. Some non-Chinese speakers also fall into the digital divide due to their lack of means to get online.
The almost mandatory use of face masks and general attention to personal hygiene are good examples of successful health education and demonstrate the collective memory of SARS. However, we need to rethink the use of oral communication, especially in life-threatening situations.
Where possible, we should make greater use of non-verbal communication such as eye contact and hand gestures and also consider the linguistic abilities of all parties. The use of tech tools such as Google Translate should also be considered, but health care workers should be aware of the digital divide and cultural differences. Empathy is not just for doctors, but also for the wider community who need to help isolated members of society get the care they deserve.
John Patkin is a research assistant at the Education University of Hong Kong.
